Spinal disc replacement is an advanced procedure used to relieve chronic back pain and restore mobility in patients with degenerative disc conditions. However, patient suitability depends on several things, and one of the most important is bone density. Adequate bone strength supports long-term implant stability and lowers the risk of complications. Dr. Larry Davidson, a specialist in spinal surgery, recognizes the importance of evaluating a patient’s full medical profile to determine the most effective treatment. As technology continues to evolve, tools like AI are helping surgeons account for key aspects of bone quality during preoperative planning.
Bone health is a foundational part of spinal surgery planning. Whether a patient has strong, healthy bones or shows signs of bone loss, understanding the condition of the spine’s supporting structures is essential for long-term implant success. Assessing and, when necessary, improving bone density can significantly influence both surgical outcomes and the recovery process.
Why Bone Density Matters
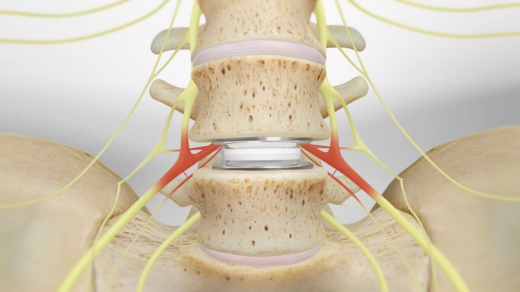
Bone density is a measure of bone strength and mineral content, which directly impacts the spine’s ability to support an artificial disc. Patients with low bone density may face challenges in achieving optimal surgical results, as weaker bones may struggle to properly integrate with the implant. Without sufficient bone strength, complications such as implant subsidence (the sinking of the artificial disc into the vertebrae) or implant loosening may occur over time.
To mitigate these risks, pre-surgical bone health assessments, including Dual-energy X-ray absorptiometry scans, can help determine a patient’s suitability for artificial disc replacement. Strengthening bone density through proper nutrition, weight-bearing exercises and supplementation may improve surgical outcomes and long-term implant stability. Addressing bone health before surgery can enhance recovery, reduce complications and improve the overall success of spinal disc replacement.
How Low Bone Density Affects Disc Replacement Outcomes
Patients with osteoporosis or osteopenia—conditions characterized by low bone density—face an increased risk of implant failure following spinal disc replacement. These conditions weaken the bones, making it harder for them to support an artificial disc and increasing the likelihood of complications such as:
• Implant subsidence: The artificial disc may sink into the weakened bone, leading to misalignment and instability.
• Vertebral fractures: Fragile bones are more prone to fractures during and after surgery.
• Delayed healing: Bone that lacks sufficient mineral density may take longer to integrate with the implant, prolonging the recovery process.
Due to these risks, patients with poor bone density may need additional treatments to improve bone strength before undergoing spinal disc replacement.
Assessing Bone Density Before Surgery
A thorough preoperative evaluation is essential for determining whether a patient’s bone density is sufficient to support spinal disc replacement. Physicians typically use Bone Mineral Density (BMD) tests, such as:
• Dual-energy X-ray absorptiometry scans: This test measures bone mineral density and helps identify osteoporosis or osteopenia.
• CT-based bone quality analysis: Provides detailed imaging of spinal structures, allowing surgeons to assess bone strength more accurately.
• MRI scans: While not a direct measure of bone density, MRI scans help evaluate overall spinal health and detect underlying conditions.
Improving Bone Density Before Surgery
For patients with low bone density, improving bone health before spinal disc replacement may enhance surgical outcomes. Physicians often recommend a combination of:
1. Calcium and Vitamin D Supplementation
o Essential for bone strength and density, calcium and vitamin D play a critical role in maintaining skeletal health.
2. Weight-Bearing Exercises
o Activities such as walking, resistance training and yoga can stimulate bone growth and density improvements.
3. Medications for Osteoporosis
o Physicians may prescribe bisphosphonates, Selective Estrogen Receptor Modulators (SERMs) or other bone-strengthening drugs to enhance bone density before surgery.
4. Lifestyle Modifications
o Avoiding smoking and limiting alcohol consumption are key factors in preventing further bone loss.
By implementing these strategies, patients can optimize their bone health, potentially improving their candidacy for spinal disc replacement.
Alternative Surgical Options for Patients with Low Bone Density
In cases where bone density is too low for spinal disc replacement, surgeons may consider alternative treatments, such as:
• Spinal fusion surgery: This procedure stabilizes the spine by permanently joining two vertebrae, eliminating the need for an artificial disc.
• Hybrid procedures: In some cases, a combination of disc replacement and fusion may be used to maintain motion while ensuring stability.
• Non-surgical treatments: Physical therapy, pain management strategies and lifestyle changes may help patients avoid surgery altogether.
Dr. Larry Davidson emphasizes, “AI will provide us with the ability to have a total and comprehensive understanding of the patient’s medical history and what sort of spinal interventions would be considered as best practices. It’s easy to envision how AI will enable us to quickly review and summarize existing medical literature regarding specific types of patients, with unique medical conditions, and their outcomes following certain spinal surgical procedures.” His statement reflects the growing role of technology and AI in spinal surgery, helping physicians make data-driven decisions tailored to each patient’s bone health, spinal condition and overall medical history.
Long-Term Impact of Bone Density on Surgical Success
Even after successful spinal disc replacement, maintaining bone density is essential for long-term stability and implant durability. Patients should follow a comprehensive post-surgical plan that includes:
• Regular bone density monitoring to detect potential changes in skeletal health.
• Physical therapy and low-impact exercises to strengthen the spine without placing excessive stress on the implant.
• A balanced diet rich in calcium, vitamin D and protein to support ongoing bone regeneration.
For older adults, managing age-related bone loss is particularly important. A decline in bone density over time can increase the risk of complications, such as adjacent segment disease, where the stress placed on neighboring vertebrae leads to further spinal degeneration.
Beyond the Implant: Prioritizing Bone Density
Bone density plays a vital role in determining the success of spinal disc replacement surgery. Patients with strong, healthy bones are more likely to achieve stable implant integration, smoother recovery and better long-term outcomes. For those with lower bone density, addressing bone health before surgery through nutrition, exercise or medication can reduce risks and improve surgical readiness.
Thorough screening, personalized planning and continued bone maintenance after surgery are essential for lasting results. With tools like AI assisting in treatment selection and bone health assessment, surgeons can better match procedures to each patient’s needs. For individuals not suited to disc replacement, alternatives such as spinal fusion may provide a safer and more effective path to relief. Prioritizing bone strength is key to ensuring a successful outcome and maintaining spinal health for years to come.